Digital Health Classification Systems
Boris Sevarika and Katarina Ceranic
Introduction to the paper “Digital Health Classification Systems” by Boris Sevarika and Katarina Ceranic
It's hard to keep track in the Digital Health Sector because there are so many stakeholders and so many startups with digital solutions as innovation drivers. Digital Health is a complex and wide-ranging field in which the players represent different interests.
As 5-HT Digital Hub Chemistry & Health, we want to match the right partners, i.e. to guide startups to their potential partners throughout the product life cycle in its entirety.
Due to the great complexity of the sector, this has been challenging so far.
To lift the fog, we have explored our own extensive digital health classification system which clusters product types according to their audience during different life cycle phases. Boris Sevarika developed this - supported by Katarina Ceranic - as part of his work for the Digital Hub.
Stefan Kohl and Dr. Frank Funke,
CEO at 5-HT Digital Hub Chemistry & Health
Digital Health Classification Systems
Authors: Boris Sevarika and Katarina Ceranic
 Katarina Ceranic and Boris Sevarika
Katarina Ceranic and Boris Sevarika1 Abstract
The startups aiming to enter the digital health market encounter various challenges. The path from the idea to the scale-up of a fully rounded product is paved with difficulty. If you are a startup looking to enter the digital health scene, you’re probably interested in knowing who would be able to support your idea either financially, logistically or who is your target user.
Different healthcare stakeholders are interested in different products and services during different stages of their life cycle. This points to the necessity of an extensive digital health classification system which clusters product types according to their audience during different life cycle phases. Each cluster should consist of different products or services that have the same end users, and, in whose development, the same stakeholders are involved.
A system like this could easily guide the startup to the suitable partners throughout the product life cycle in its entirety. However, the 5-HT Digital Hub Chemistry & Health found that the existing categorization systems obscure the partners from the startup and have therefore, in this work, explored a novel classification system of our own design which allows startups and healthcare stakeholder to find each other more quickly and easily.
2 Table of Contents
1. Abstract
2. Table of Contents.
3. Digital Health Today.
4. Healthcare Sector Complexity.
5. Digital Health Startups as Innovation Drivers.
6. Importance of Cooperation.
7. Finding the Right Partner.
8. Existing Digital Health Classification Systems.
8.1 World Health Organization.
8.2 Federal Drug Administration.
8.3 The Digital Healthcare Act.
8.4 Classification According to Maximilian Herrmann.
9. Existing Categorization Methods Disadvantages.
10. Proposed Categorization System.
11. Conclusion.
12. References.
3 Digital Health Today
Digital Health or eHealth is an umbrella term. Digital Health incorporates the use of a wide range of information and communication technologies intended to reform and upgrade public health and health care system (Fadahunsi et al., 2019; Piette et al., 2012). It employs different hardware and software tools such as mobile phones, sensor technologies and other monitoring tools as well as data analyzing programs (Turakhia et al., 2016).
While many digital health tools are used mostly by the patients, their physicians and pharmacists, some of them have proved invaluable for the pharmaceutical industry, medical institutions as well as health insurance companies (Fadahunsi et al., 2019). Digital Health is a pioneer in providing easily accessible personalized high-quality healthcare (Fadahunsi et al., 2019). It gathers objective data which is accessible to both the patient and the caregiver leading to a transparent and shared decision-making process (Meskó et al., 2017).
As the deficiency in trained medical staff is becoming more apparent and the healthcare system fails to appropriately respond to the patients’ needs, the impending paradigm shift is ever closer (Meskó et al., 2017). We advocate for the use of disruptive innovations through small business startup projects to start the comprehensive change in the overall system.
4 Healthcare Sector Complexity
The healthcare sector shows high complexity. Many traditional stakeholders are involved – the pharmaceutical industry, medical institutions, insurance providers, physicians, rehabilitation centers, nursing homes, distributors, and the patients themselves. Different stakeholders solicit different solutions customized to their particular needs. Some stakeholders are responsible for the research and development of the new products, some are primarily financiers, while others are the end users of said products and services.
These various stakeholders are all interested in the digitalization of healthcare. Their incentives and goals are diverse, which is why all of them have different digitalization approaches. While the hospitals and clinics invest principally in patient-centered infrastructures in order to enhance the user experience (Gomes and Romão, 2015), the pharmaceutical industry is more interested in establishing new research and development tools to accelerate the development processes as well as new digital products and services for other healthcare stakeholders.
5 Digital Health Startups as Innovation Drivers
The importance of data analysis and manipulation in medicine has increased during the past decades. One of the many examples of the revolutionary digital health technologies are the picture recognition algorithms utilizing artificial intelligence used in the cancer diagnostics (Weiss et al., 2020). Furthermore, artificial intelligence-based software tools have been successfully employed in screening for diabetic retinopathy (Ting et al., 2020). Ting even states that the artificial intelligence performs better in the tests compared to experienced medical professionals.
Millions of different smart devices are collecting huge amounts of data every day. Their aggregation and integration into the existing infrastructure systems could break new ground in the field of preventive medicine.
The emerging importance of these and other cutting-edge technologies is being especially recognized in the startup scene. The startups are entrepreneurial ventures that lend themselves to identifying the problem existing within the established system and offering solutions that seamlessly blend into it. They are agile, driven and highly motivated (Weiblen and Chesbrough, 2015). While digital health startups can be a threat for some healthcare stakeholders, for others, they are an inspiration. The majority of the healthcare enterprises see the startups as an opportunity to spark their own digital evolution (Rinsche, 2017).
6 Importance of Cooperation
The startups and the corporates have different needs. While many newly founded startups require investments, additional expertise in specific fields or broader market access, big companies need inventive ideas and their prompt implementation. The corporations possess resources, robustness and the ability to scale. Their routines and developed internal processes run their established business model efficiently (Weiblen and Chesbrough, 2015).
On the other hand, the complex organizational structure and decision-making processes slow down the adoption and setting up of disruptive technologies. Startups can react to the market requirements fast and adapt to the new environments quickly. Each side has exactly what the other one does not (Weiblen and Chesbrough, 2015). To achieve overall system harmony and functionality as well as a readiness in tackling new challenges, cooperation is crucial.
Startups undergo different cooperation arrangements when developing and launching their product. Each arrangement is primarily driven by the common interests of the parties involved. Hence, it is essential for the startup to correctly identify suitable partners each step of the way. Firstly, in the development phase, pinpointing the establishment working on related projects is challenging in its own right. After defining the minimal viable product and preparing it for the market entry, the relationships with the customers start to play an important role. When scaling up, optimizing the product or service according to the user feedback should stay in focus. The users generate considerable amounts of data valuable to many shareholders, so the startup has to be aware of who would benefit from gaining access to said data.
7 Finding the Right Partner
Each product goes through several phases during its life cycle – the development phase, the market entry phase and the scale-up phase. The startups face peculiar challenges during each phase and to overcome them they enter partnerships and cooperation accordingly.
Different healthcare stakeholders are interested in different types of digital health products and services. A particular product type is going to interest various partners during its life cycle phases. While one partner could be interested in the product co-development, another may want to partake in the marketing and distribution whereas others can be labeled as the end users. Some associates could be interested in cooperation throughout the whole life cycle, when some would not be interested at all in that product type.
Therefore, the startup should be aware of the product type it is developing and its classification so that it would be able to determine the suitable potential partners in each life cycle phase easily. This points to the necessity of an extensive digital health classification system which clusters product types according to their audience during different life cycle phases. Each cluster consists of different products or services that have the same end users, and, in whose development, the same stakeholders are involved. Currently, various digital health classification systems are in use.
8 Existing Digital Health Classification Systems
8.1 World Health Organization
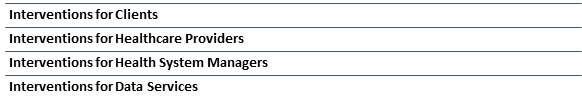
The World Health Organization (World Health Organization, 2018) has presented a classification based on the categorization of digital health interventions. This system is primarily targeted at the public health policy makers and its objective is to explore the prospects of the digital infrastructure development. There are four major classification categories.
The first three are focused on the interventions aimed towards the digitalization of the existing healthcare system services for different end users. They include interventions for clients, interventions for healthcare providers and interventions for health system managers. The fourth category encompasses the interventions aimed towards collecting, structuring and processing of data.
However, this categorization completely overlooks the use and integration of the newest technologies used in the healthcare sector such as the previously mentioned artificial intelligence-based cancer diagnostics software or the picture recognition diabetic retinopathy screening tools.
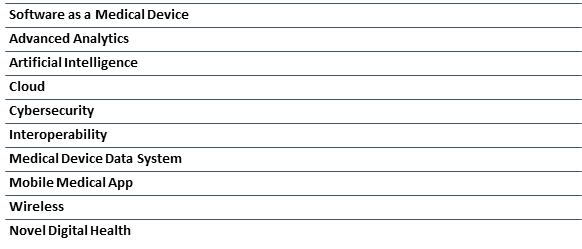
8.2 Federal Drug Administration
The Federal Drug Administration defines the digital health subgroups based on the technology used in each product or service. This classification describes the legal regulations a product must adhere to in order to be marketed depending on the technology it implements. Nevertheless, these criteria do not offer a clarification on what purpose each product serves.
8.3 The Digital Healthcare Act
The Digital Healthcare Act of the German Federal Government tends to the needs and expectations of the patient. It explores the digital health applications designed for the patient and neglects the other aspects of digital healthcare.
As such, it distinguishes between the solutions that have a structural and procedural effect on the patient and the products that have medical benefits. Among the specified structural and procedural effects are access to care, securing the standard of care, health literacy and adherence to the therapy plan. The stated medical benefits are increased quality of life and lowered morbidity and mortality.
8.4 Classification According to Maximilian Herrmann
Maximilian Herrmann et al. analyzed over 400 different digital health projects and solutions and classified them according to their purpose into six different categories (Herrmann et al., 2018).
The proposed categorization considers digital health solutions aimed towards patients and healthcare providers and does not focus on the products and services aimed towards other healthcare stakeholders such as insurance companies or pharmaceutical industry.
9 Existing Categorization Methods Disadvantages
The presented digital health classification systems have been devised with a particular purpose in mind and as such are not applicable out of the original context of use.
The World Health Organization designed its classification system for the healthcare policy makers. The main aim was devising the nomenclature used in the digitalization of healthcare. This categorization omits parts of the contemporary digital health sector and focuses on the infrastructure of the digitalization in the traditional healthcare sector. This along with the fact that it completely disregards the modern technologies and the products based on them renders this categorization inadequate.
The Federal Drug Administration is the American regulatory authority for drugs and medical products. It concentrates on the technologies employed in the product creation and the product overall safety to humans. This classification system overlooks the product applications and cannot be consulted in the search for the appropriate partners.
The German Government focuses on the patient and how each product affects them. The categorization is based on the types of benefits a product has on the patient. As it is not exhaustive enough it cannot be used to easily identify potential collaborators.
Maximilian Herrmann et al. established a classification on the actual products designed by the startups and industry already in the market. This categorization is based on the purposes and scopes of application and portrays a realistic picture of the various products. However, the authors analyzed only the products aimed towards the patients and the healthcare professionals disregarding the products designed for the industry, the insurance companies and other stakeholders.
10 Proposed Categorization System
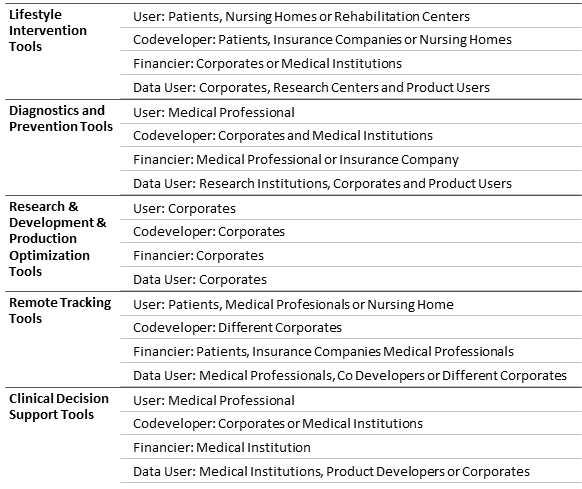
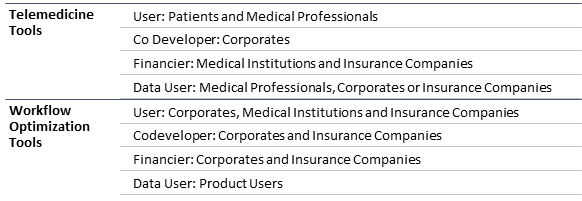
The proposed categorization system heavily relies on the classification suggested by Maximillian Herrmann et al. with some improvements and upgrades. The categories Lifestyle Intervention Tools and Diagnostics and Prevention Tools were assumed form the Herrmann classification. We also added the category Research & Development & Production Optimization Tools which covers the digital health solutions aimed towards application in the industrial settings.
The Herrmann classification originated in analyzing the actual concurrent projects in the field of digital health. It does not include aspects of digital health such as infrastructure related solutions and telemedicine tools which have entered the market some time ago. Moreover, the further aspects of digital health that have been overlooked are clinical decision support solutions as well as patient tracking systems. Thus, we introduced the categories Remote Tracking Tools, Clinical Decision Support Tools, Telemedicine Tools and Workflow Optimization Tools.
11 Conclusion
In this paper we provided a definition of the digital health and touched on the complexity of the healthcare system. We identified the different roles in the system – the healthcare users, the service providers, the manufacturers, the distributors and the other market players.
The role of the startups as the primary agent of innovation was discussed as well as the importance of employing the cutting-edge technologies. This was followed by an analysis on the influence of cooperation between the startups and the established organizations and the examples of cooperation models. We pinpointed the difficulties searching for the appropriate partner entails.
After that, we stated that digital health products and services can be clustered into different groups according to specific similarities and explained how classification systems can be employed when roughly determining key associates depending on the product type. We explored the existing categorization systems and listed their advantages and disadvantages. The overall impression was that these systems obscured the partners from the startup rather than highlighting them.
Later, we proposed our own
categorization system which clusters products according to their audience
during different life cycle phases. We firmly believe that our proposed
categorization criteria would enable startups to find the fitting partners as effortlessly
as possible.
12 References
Fadahunsi, K.P., Akinlua, J.T., O’Connor, S., Wark, P.A., Gallagher, J., Carroll, C., Majeed, A., O’Donoghue, J., 2019. Protocol for a systematic review and qualitative synthesis of information quality frameworks in eHealth. BMJ Open 9. https://doi.org/10.1136/bmjopen-2018-024722
Gomes, J., Romão, M., 2015. The success of IS/IT projects in the healthcare sector: Stakeholders’ perceptions. 2015 10th Iberian Conference on Information Systems and Technologies, CISTI 2015. https://doi.org/10.1109/CISTI.2015.7170516
Herrmann, M., Boehme, P., Mondritzki, T., Ehlers, J.P., Kavadias, S., Truebel, H., 2018. Digital transformation and disruption of the health care sector: Internet-based observational study. Journal 0f Medical Internet Research 20, 104–112. https://doi.org/10.2196/jmir.9498
Meskó, B., Drobni, Z., Bényei, É., Gergely, B., Győrffy, Z., 2017. Digital health is a cultural transformation of traditional healthcare. mHealth 3, 38–38. https://doi.org/10.21037/mhealth.2017.08.07
Piette, J.D., Lun, K.C., Moura, L.A., Fraser, H.S.F., Mechael, P.N., Powellf, J., Khoja, S.R., 2012. Impacts of e-health on the outcomes of care in low- and middle-income countries: where do we go from here? Bulletin of the World Health Organization 90, 365–372. https://doi.org/10.2471/BLT.11.099069
Rinsche, F., 2017. The Role of Digital Health Care Startups. Crossing Borders - Innovation in the U.S. Health Care System 84, 185–195.
Ting, D.S.W., Lin, H., Ruamviboonsuk, P., Wong, T.Y., Sim, D.A., 2020. Artificial intelligence, the internet of things, and virtual clinics: ophthalmology at the digital translation forefront. The Lancet Digital Health 2, e8–e9. https://doi.org/10.1016/S2589-7500(19)30217-1
Turakhia, M.P., Desai, S.A., Harrington, R.A., 2016. The outlook of digital health for cardiovascular medicine: Challenges but also extraordinary opportunities. JAMA Cardiology 1, 743–744. https://doi.org/10.1001/jamacardio.2016.2661
Weiblen, T., Chesbrough, H.W., 2015. Engaging with startups to enhance corporate innovation. California Management Review 57, 66–90. https://doi.org/10.1525/cmr.2015.57.2.66.
Weiss, J., Hoffmann, U., Aerts, H.J.W.L., 2020. Artificial intelligence-derived imaging biomarkers to improve population health. The Lancet Digital Health 2, e154–e155. https://doi.org/10.1016/S2589-7500(20)30061-3
World Health Organization, 2018. Classification of digital health interventions v1.0 A shared language to describe the uses of digital technology for health, World Health Organization. Geneva.
5-HT Chemistry & Health Newsletter
Want the latest tech and industry news, events, relevant info from the ecosystem and more?
Subscribe to 5-HT Newsletter now Subscribe to 5-HT Newsletter now
Become part of the 5-HT Chemistry & Health
Exchange ideas with innovative startups and future-oriented companies in our ecosystem. We look forward to meeting you!